Joint Mobilisation: Beyond Stiffness
Joint mobilisation, a therapeutic technique employed by healthcare professionals, has long been associated with addressing stiffness and improving joint flexibility.
However, the benefits of joint mobilisation extend far beyond merely alleviating stiffness. This article delves into the transformative effects of joint mobilisation on range of motion, exploring its physiological mechanisms, clinical applications, and the evidence supporting its efficacy.
Understanding Joint Mobilisation
Joint mobilisation is a manual therapy technique used by practitioners to address restrictions in joint movement. It involves the skilled manipulation of joints and surrounding tissues to enhance their mobility and function. While often used in the context of musculoskeletal disorders, joint mobilisation has broader applications, playing a crucial role in rehabilitation and performance enhancement.
Physiological Mechanisms
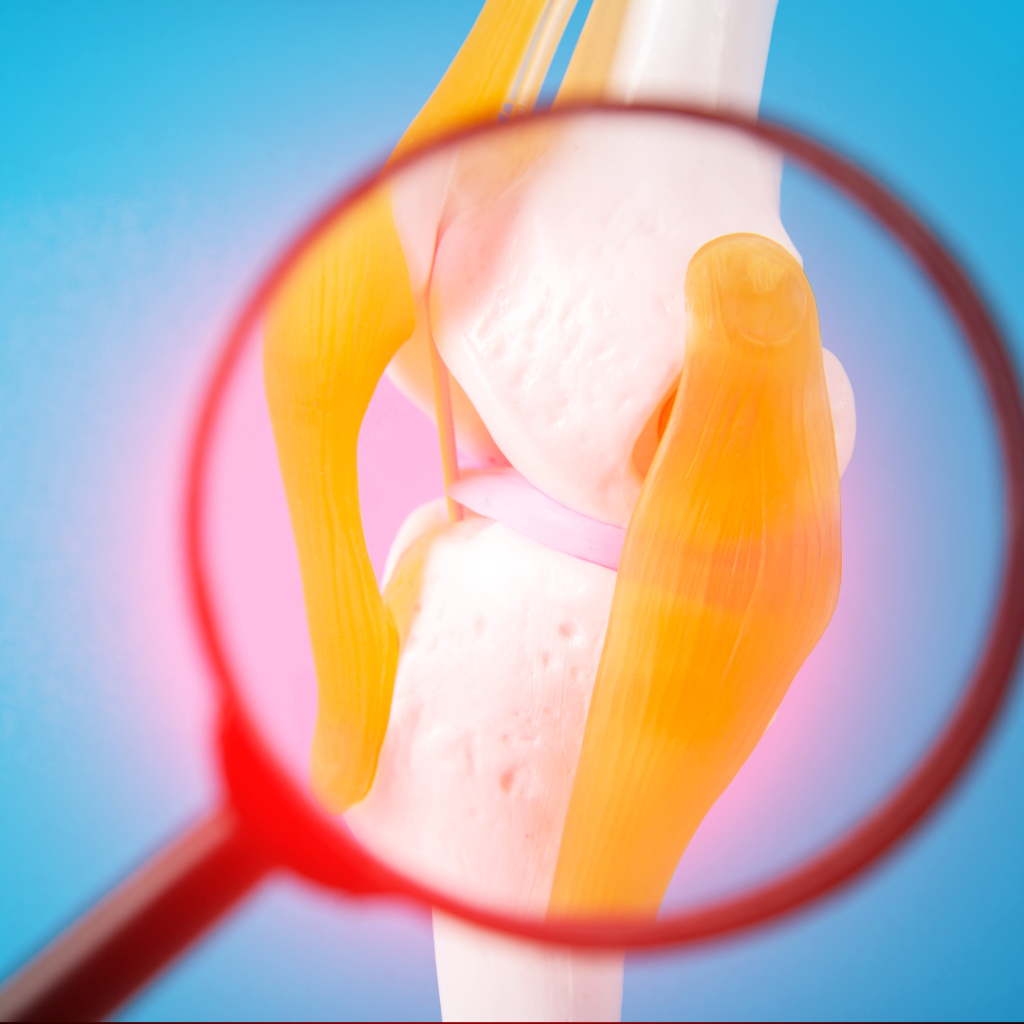
To comprehend how joint mobilisation transforms range of motion, it is essential to delve into the physiological mechanisms at play. Joint mobilisation primarily targets the connective tissues surrounding the joint, including ligaments, joint capsules, and the synovial membrane. These structures are rich in mechanoreceptors, which respond to mechanical stimuli.
1. Stretching of Connective Tissues:
Joint mobilisation induces controlled stretching of the connective tissues, leading to a temporary increase in their length. This stretching stimulates mechanoreceptors, sending signals to the central nervous system. The nervous system, in turn, responds by modulating muscle tone and promoting relaxation, facilitating improved joint mobility.
2. Synovial Fluid Distribution:
The synovial fluid within joints serves as a lubricant and a source of nutrition for the joint structures. Joint mobilisation promotes the even distribution of synovial fluid, enhancing joint lubrication and reducing friction. This lubrication aids in smoother joint movements, positively impacting range of motion.
3. Neuromuscular Effects:
Joint mobilisation influences the neuromuscular system by modulating the activity of motor neurons and muscle spindle fibres. This leads to a reduction in muscle stiffness and an improvement in muscle flexibility, contributing to enhanced joint mobility.
Clinical Applications
Joint mobilisation finds widespread application in various clinical settings, addressing a spectrum of musculoskeletal issues and contributing to overall well-being.
1. Orthopaedic Rehabilitation:
Following surgeries, fractures, or joint injuries, joint mobilisation is often incorporated into rehabilitation programs to restore normal joint function. It helps break down scar tissue, improve flexibility, and prevent the development of adhesions that could limit range of motion.
2. Sports Medicine
Athletes frequently utilise joint mobilisation as a preventive and rehabilitative measure. Regular joint mobilisation sessions can enhance joint flexibility, reduce the risk of injuries, and promote optimal athletic performance.

3. Chronic pain management
Individuals suffering from chronic pain conditions, such as osteoarthritis or fibromyalgia, may benefit from joint mobilisation. By addressing stiffness and improving range of motion, joint mobilisation contributes to pain relief and enhanced functional capacity.
4. Geriatric Care
In the elderly population, joint mobilisation is valuable for maintaining joint health and preventing age-related stiffness. It can be particularly beneficial for individuals with conditions like osteoporosis, promoting mobility and reducing the risk of falls.
Efficacy and Evidence
The effectiveness of joint mobilisation is supported by a growing body of research across diverse populations and conditions.
1. Osteoarthritis
A study published in the “Journal of Orthopaedic & Sports Physical Therapy” found that joint mobilisation significantly improved pain, stiffness, and physical function in individuals with knee osteoarthritis. The results highlighted the potential of joint mobilisation as a non-pharmacological intervention for managing osteoarthritic symptoms.
2. Post-Surgicial Rehabilitation
Research in the “Archives of Physical Medicine and Rehabilitation” demonstrated the benefits of joint mobilisation in post-surgical rehabilitation. Patients undergoing joint mobilisation after total knee arthroplasty showed improved range of motion and reduced pain compared to those receiving conventional physiotherapy alone.
3. Athletic Performance
In the realm of sports science, a systematic review published in the “Journal of Science and Medicine in Sport” concluded that joint mobilisation has positive effects on range of motion and muscle performance. Athletes incorporating joint mobilisation into their training regimens exhibited enhanced flexibility, contributing to improved sports performance.
TYPES OF JOINT MOBILISATIONS
There are several types of joint mobilisations, each with its own specific characteristics and indications. Here are some common types:
1. Grade I Mobilisation (Joint Oscillation):
Description: Involves small, rhythmic oscillations at the beginning of the joint’s available range. The movements are gentle and within the patient’s pain-free range.
Indications: Suitable for reducing pain, initiating joint movement, and promoting relaxation.
2. Grade II Mobilisation (Joint Mobilisation with Reduced Range):
Description: This technique involves larger oscillations than Grade I, targeting a slightly greater range of joint motion. The therapist applies controlled force within the patient’s pain-free range.
Indications: Useful for increasing joint mobility, reducing muscle guarding, and improving joint nutrition.
3. Grade III Mobilisation (Joint Mobilisation to End Range):
Description: In Grade III mobilisation, the joint is mobilised up to its end range, but not beyond. The therapist applies a moderate force to stretch the joint capsules and surrounding tissues.
Indications: Effective for increasing joint range of motion and addressing joint stiffness.

4. Grade IV Mobilisation (Joint Mobilisation beyond End Range):
Description: This technique involves taking the joint beyond its anatomical end range. The therapist applies a firm force to stretch tight structures, but it should be done cautiously to avoid injury.
Indications: Used sparingly for specific joint restrictions and stubborn joint stiffness.
5. Grade V Mobilisation (Manipulation or Thrust Techniques):
Description: Grade V mobilisation involves a quick, high-velocity thrust at the end of the joint’s range. This technique is often referred to as joint manipulation.
Indications: Reserved for specific joint dysfunctions, it is effective in cases where other mobilisation grades may not be sufficient.
6. Accessory Mobilisation:
Description: Involves mobilising specific joint structures, such as joint capsules or ligaments, rather than moving the joint through its entire range.
Indications: Useful for addressing specific restrictions within joint structures.
7. COMBINED MOVEMENTS:
Description: This technique combines passive movements in different planes to address multi-planar joint restrictions. Therapists use a combination of gliding, rolling, and spinning motions.
Indications: Effective for addressing complex joint restrictions involving multiple movement planes.
IN CONCLUSION:
Joint mobilisation goes beyond addressing stiffness; it is a transformative therapeutic technique with profound effects on range of motion. By targeting the physiological mechanisms underlying joint function, this manual therapy modality proves valuable across diverse clinical applications.
From orthopaedic rehabilitation to sports medicine and geriatric care, the evidence supporting the efficacy of joint mobilisation is compelling. Healthcare professionals should continue to explore and refine the application of joint mobilisation, unlocking its full potential to enhance joint mobility, improve functional outcomes, and contribute to the overall well-being of individuals across the lifespan.
If you wish to seek further help or speak to a practitioner about any of the above, call us on 0800 731 2738 or book online here.
You can also view all the services we provide within our clinics on our website, as well as checking out our other blogs and content.
For more free tips and information, make sure to follow our Facebook and Instagram pages. We also post client stories, so you can see how we’ve helped people get back to doing the things they enjoy!